Today we look at the condition Plantar Fasciitis. Chartered Physiotherapist Fiona Casey, explains what the condition is, how it occurs and how it can be treated. So to fully understand what plantar fasciitis is, we must first look at the plantar fascia….
So what is the plantar fascia?
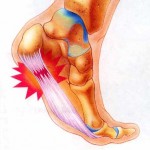
The plantar fascia is made up of a thick connective or fibrous tissue that helps to form and support the sole and the arch of the foot. It runs from its origin at the heel bone forward along the sole of the foot to each of the five toes.
In the younger person, the plantar fascia continues from the heel to the Achilles tendon, and therefore the Achilles tendon can become painful and problematic in some instances of plantar fasciitis. Plantar fasciitis is a common foot condition which can cause heel pain and pain into the sole of the foot. It can be worse first thing in the morning or following a period of rest. The pain can be eased with walking, as walking stretches or mobilises the sole of the foot.
So what causes plantar fasciitis?
The pathology is believed to be secondary to the development of microtrauma or microtearing within the connective tissue that forms the plantar fascia. These microtears, normally occur as a result of excessive stress or stretching of the plantar fascia in weight bearing positions.
The resulting inflammatory condition is actually from a degenerative process within the plantar fascia. The key to effective treatment of plantar fasciitis is to identify the source of the inflammation and address this problem. Often plantar fasciitis can occur for no specific reason, however certain factors can increase the risk of this condition developing,
- Restriction in the calf muscle or Achilles sometimes post injury can lead to changes in stresses and tension through the plantar fascia
- A notable weight gain can also lead to changes in pressure and stress through the foot with weight bearing activities.
- An unaccustomed or repetitive activity / increased training over a short period of time on uneven surfaces.
- Wearing flat unsupportive footwear on hard surfaces can place abnormal stress through the plantar fascia as can changing from a high heeled to a flat-soled shoe.
Who gets plantar fasciitis?
Plantar fasciitis is commonly found in middle-aged people. It can affect anyone who is on their feet a lot, like athletes, nurses, soldiers and shop assistants.
What are the symptoms of plantar fasciitis?
- Pain in the heel or sole of the foot with weight bearing activities
- Pain with walking, standing or after exercise
- Typically pain is noted to be most severe first in the morning and gradually subsides with walking, as walking stretches the plantar fascia.
- Pain can be felt as a burning or sharp sensation and can radiate into the Achilles tendon if severe.
So how is this condition treated?
In the initial acute stages of plantar fasciitis, conservative management is favorable
REST: You will be advised to rest from aggravating factors such as high impact or high load exercise. Low load exercise is normally encouraged, such as swimming, and cycling.
ICE: You will be advised by your chartered physiotherapist to try local icing to the heel and sole of the foot.
Anti-inflammatory medication: May have a role in the initial stages of treatment, however it will be best to discuss this option with your GP, as long term anti-inflammatory medication may have a limited effect.
EXERCISE: Your chartered physiotherapist will best advise you on suitable exercise for your specific symptoms. It is important to mobilise the healing plantar fascia in order to promote a healthy blood supply to the connective tissue.
Chartered physiotherapists will also advise you on shoe modification including adequate cushioning and support to offload the plantar fascia and provide a supportive environment for the foot.
You may also be advised with relation to
- strapping techniques
- Orthotic devices, initially a temporary device may be used to provide a structured support for the plantar fascia and offload the connective tissue in the healing phases.
- Assessment of the knee and hip muscles to ensure adequate lower limb support and motion control.
- A Rehabilitative programme of strengthening exercises for the lower limb in order to prevent the condition returning.
- Specific Advice with relation to returning to your sport or exercise routine.